The World Health Organization defines health as a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.
Healthcare industry comprises hospitals, medical devices, clinical trials, outsourcing, telemedicine, medical tourism, health insurance and medical equipment.
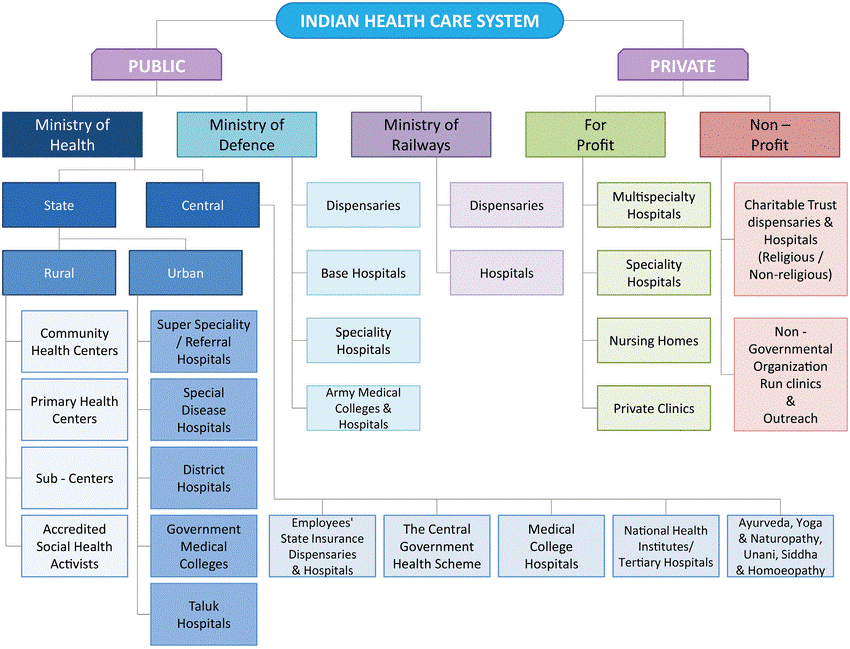
At present, India’s health care system consists of a mix of public and private sector providers of health services. Networks of health care facilities at the primary, secondary and tertiary level, run mainly by State Governments, provide free or very low-cost medical services. There is also an extensive private health care sector, covering the entire spectrum from individual doctors and their clinics, to general hospitals and super speciality hospitals.
Problems pertaining to Healthcare sector in India
Insufficient Medical personnel:
- There is a massive shortage of medical staff, infrastructure and last mile connectivity in rural areas. g.: Doctor: Population 1:1800 and 78% doctors cater to urban India (population of 30%).
- Massive shortages in the supply of services (human resources, hospitals and diagnostic centres in the private/public sector) which are made worse by grossly inequitable availability between and within States.
- For example, even a well-placed State such as Tamil Nadu has an over 30% shortage of medical and non-medical professionals in government facilities.
- 61% PHCs have just one doctor, while nearly 7% are functioning without any
- 33% of PHCs do not have a lab technician, and 20% don’t have a pharmacist.
- In states like Odisha, more than 3,000 government posts for doctors or about 50% of all government medical doctor posts are lying vacant.
Health budget:
- India’s expenditure on the health sector has risen meagerly from 1.2 per cent of the GDP in 2013-14 to4 per cent in 2017-18. The National Health Policy 2017 had aimed for this to be 2.5% of GDP.
- The health budget has neither increased in real terms nor is there any policy to strengthen the public/private sector in deficit areas. While the Ayushmaan Bharat provides portability, one must not forget that it will take time for hospitals to be established in deficit areas.
- This in turn could cause patients to gravitate toward the southern States that have a comparatively better health infrastructure than the rest of India.
Infrastructure constraints:
- There are doubts on the capacity of India’s infrastructure to take on the additional load of patients during pandemics like Covid-19 as seen recently.
- There is a growing medical tourism (foreign tourists/patients) as a policy being promoted by the government, and also domestic patients, both insured and uninsured.
Crumbling public health infrastructure:
- Given the country’s crumbling public healthcare infrastructure, most patients are forced to go to private clinics and hospitals.
- There is a shortage of PHCs (22%) and sub-health centres (20%), while only 7% sub-health centres and 12% primary health centres meet Indian Public Health Standards (IPHS) norms.
- In the northern States there are hardly any sub-centres and primary health centres are practically non-existent. First mile connectivity to a primary healthcare centre is broken. For eg, in Uttar Pradesh there is one PHC for every 28 villages.
Strong role of Private players:
- Approximately 70 per cent of the healthcare services in India are provided by private players. If private healthcare crumbles due to economic constraints or other factors, India’s entire healthcare system can crumble.
- Over 70 per cent of the total healthcare expenditure is accounted for by the private sector.
- However, Private hospitals don’t have adequate presence in Tier-2 and Tier-3 cities and there is a trend towards super specialisation in Tier-1 cities.
- lack of transparency and unethical practices in the private sector.
- Lack of level playing field between the public and private hospitals has been a major concern as public hospitals would continue receiving budgetary support. This would dissuade the private players from actively participating in Governmental scheme.
High Out of pocket expenditure:
- According to the latest National Health Accounts (NHA) estimates released in March 2021, patients bear a big chunk of health expenses, as high as 61 per cent of the total health expenditure, by themselves.
- Even the poor are forced to opt for private healthcare, and, hence, pay from their own pockets. As a result, an estimated 63 million people fall into poverty due to health expenditure, annually.
- Inequities in the health sector exist due to many factors like geography, socio-economic status and income groups among others. Compared with countries like Sri Lanka, Thailand and China, which started at almost similar levels, India lags behind peers on healthcare outcomes.
Poor insurance penetration:
- India has one of the lowest per capita healthcare expenditures in the world. Government contribution to insurance stands at roughly 32 percent, as opposed to 83.5 percent in the UK.
- The high out-of-pocket expenses in India stem from the fact that 76 percent of Indians do not have health insurance.
Fake doctors:
- Rural medical practitioners (RMPs), who provide 80% of outpatient care, have no formal qualifications for it.
- People fall prey for quacks, often leading to grave disabilities and loss of life.
Numerous Schemes and its limitations:
- The Government has launched many policies and health programmes but success has been partial at best.
- The National Health Policy(NHP) 2002 proposed to increase Government spending on health by two to three per cent of the gross domestic product (GDP) by 2010 which has not happened yet.
- Now, the National Health Policy 2017, has proposed to take it to 2.5 per cent of the GDP by 2025.
- The overall situation with the National Health Mission, India’s flagship programme in primary health care, continues to be dismal.
- The NHM’s share in the health budget fell from 73% in 2006 to 50% in 2019 in the absence of uniform and substantial increases in health spending by States.
Healthcare without holistic approach:
- There are a lot of determinants for better health like improved drinking water supply and sanitation; better nutritional outcomes, health and education for women and girls; improved air quality and safer roads which are outside the purview of the Health Ministry.
Issues in particular with Urban healthcare
- Rural-urban disparity: Until recently, Union government mostly focused on rural healthcare. Ex: expenditure on urban areas was ₹850 crore in 2019-20, compared to nearly ₹30,000 crore for rural.
- Lack of government primary and preventive health infrastructure: Against a norm-based target of 9,072 urban primary health centres (UPHCs), only 5,190 are operational.
- Most states do not have urban sub-centres (SCs), people’s first point of access for healthcare services. There are only 3,000 urban SCs compared to over 150,000 in rural areas.
- Urban areas also suffer from ‘over-hospitalization’ of basic care, ideally done in clinics.
- Lack of devolution of functions by state governmentand inadequate role clarity among various health-related agencies
- Poor financial condition of ULBs, and low priority accorded to health.
Issues in particular with Rural healthcare
- Only 11% sub-centres, 13% Primary Health Centres (PHCs) and 16% Community Health Centres (CHCs) in rural India meet the Indian Public Health Standards (IPHS).
- Only one allopathic doctor is available for every 10,000 people and one state run hospital is available for 90,000 people.
- Innocent and illiterate patients or their relatives are exploited, and they are allowed to know their rights.
- Most of the centres are run by unskilled or semi-skilled paramedics and doctor in the rural setup is rarely available.
- Patients when in emergency sent to the tertiary care hospital where they get more confused and get easily cheated by a group of health workers and middlemen.
- Non-availability of basic drugs is a persistent problem of India’s rural healthcare.
- In many rural hospitals, the number of nurses is much less than required.
Central Government Schemes for Healthcare Sector in India
Health is a state subject, the Central Government supplements the efforts of the State Governments in delivery of health services through various schemes for primary, secondary, and tertiary care.
- By 2025, the Government of India is planning to increase the expenditure on Health care to 2.5% of the GDP.
- In the Union Budget 2020-21, the Ministry of Health and Family Welfare was allocated a budget of more than Rs 65,000 crores.
- In Budget 2020-21, Government of India has approved the extension of National Health Mission with an allocated budget of around Rs 34,000 crores.
- Under the National Health Mission (NHM), financial support is provided in the following areas: ASHAs workers, ambulances, mobile medical units (MMUs), drugs and equipments, support for Reproductive, Maternal, New-born, Child & Adolescent Health (RMNCH+A).
- The National Nutrition Mission has set an objective of reducing the under nutrition, problems of stunting by 2%
- The Ayushman Bharat – Pradhan Mantri Jan Arogya Yojana (PMJAY) – This is the largest health care program funded by the Government.
- In the Union Budget 2020-21, PMJAY was allocated a budget of more than Rs 6400 crores.
- As of Nov 2019, more than 63 lakh people have received free treatment under Ayushman Bharat – PMJAY.
- In the Union Budget 2020-21, Government of India allocated Rs 3,000 crores for Pradhan Mantri Swasthya Suraksha Yojana (PMSSY).
Measures needed in health sector in India
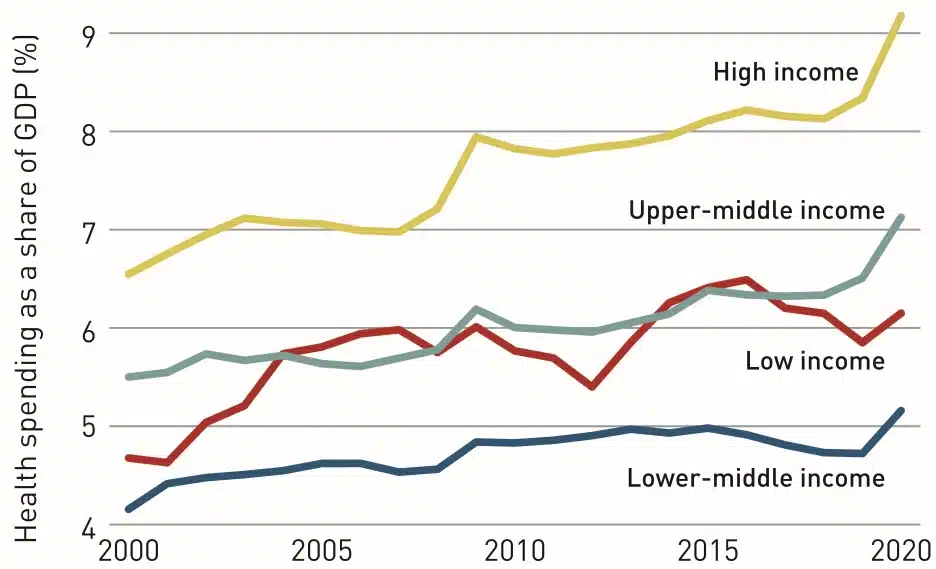
- There is an immediate need to increase the public spending to 2.5% of GDP, despite that being lower than global average of 5.4%.
- The achievement of a distress-free and comprehensive wellness system for all hinges on the performance of health and wellness centers as they will be instrumental in reducing the greater burden of out-of-pocket expenditure on health.
- there is a need to depart from the current trend of erratic and insufficient increases in health spending and make substantial and sustained investments in public health over the next decade.
- A National Health Regulatory and Development Framework needs to be made for improving the quality (for example registration of health practitioners), performance, equity, efficacy and accountability of healthcare delivery across the country.
- Increase the Public-Private Partnerships to increase the last-mile reach of healthcare.
- Generic drugs and Jan Aushadi Kendras should be increased to make medicines affordable and reduce the major component of Out of Pocket Expenditure.
- The government’s National Innovation Council, which is mandated to provide a platform for collaboration amongst healthcare domain experts, stakeholders and key participants, should encourage a culture of innovation in India and help develop policy on innovations that will focus on an Indian model for inclusive growth.
- India should take cue from other developing countries like Thailand to work towards providing Universal Health Coverage. UHC includes three components: Population coverage, disease coverage and cost coverage.
- Leveraging the benefits of Information Technology like computer and mobile-phone based e-health and m-health initiatives to improve quality of healthcare service delivery. Start-ups are investing in healthcare sector from process automation to diagnostics to low-cost innovations. Policy and regulatory support should be provided to make healthcare accessible and affordable.
Way forward
- India needs a holistic approach to tackle problems in healthcare industry.
- This includes the active collaboration of all stakeholders viz. public, private sectors, and individuals.
- There is an immediate need to increase the public spending to 2.5% of GDP, despite that being lower than global average of 5.4%.
- The achievement of a distress-free and comprehensive wellness system for all hinges on the performance of health and wellness centers as they will be instrumental in reducing the greater burden of out-of-pocket expenditure on health.
- There is a need to depart from the current trend of erratic and insufficient increases in health spending and make substantial and sustained investments in public health over the next decade.
- A National Health Regulatory and Development Framework needs to be made for improving the quality (for example registration of health practitioners), performance, equity, efficacy and accountability of healthcare delivery across the country.
- Increase the Public-Private Partnerships to increase the last-mile reach of healthcare.
- Generic drugs and Jan Aushadi Kendras should be increased to make medicines affordable and reduce the major component of Out of Pocket Expenditure.
- The government’s National Innovation Council, which is mandated to provide a platform for collaboration amongst healthcare domain experts, stakeholders and key participants, should encourage a culture of innovation in India and help develop policy on innovations that will focus on an Indian model for inclusive growth.
- India should take cue from other developing countries like Thailand to work towards providing Universal Health Coverage. UHC includes three components: Population coverage, disease coverage and cost coverage.
- Leveraging the benefits of Information Technology like computer and mobile-phone based e-health and m-health initiatives to improve quality of healthcare service delivery. Start-ups are investing in healthcare sector from process automation to diagnostics to low-cost innovations. Policy and regulatory support should be provided to make healthcare accessible and affordable.
- Leveraging AYUSH services in non-critical care as demonstrated during the pandemic can be vital to augment the capacity of the allopathic services.
- A more dynamic and pro-active approach is needed to handle the dual disease burden.
- A universal access to health makes the nation fit and healthy, aiding better to achieve the demographic dividend.
